eople are now starting to suspect that committing economic hara-kiri in the hopes of
slowing the Wuhan coronavirus may not have been such a hot idea after all.
eople are now starting to suspect that committing economic hara-kiri in the hopes of
slowing the Wuhan coronavirus may not have been such a hot idea after all.
The challenge we'll face is that no government program ever really ends. We're still defending Europe against an adversary that hasn't existed for 31 years. If the US government goes through with their plans for 2T of helicopter money, the true legacy of this virus could well be destruction of the US dollar.
The graph that almost killed America's economy
The strategy of sequestering people is not to prevent infections, but to spread the deaths out over a longer time period. This was clearly shown by the CDC's famous graph, which showed that the area under the two curves—sequestered and non-sequestered—was the same. The goal was to keep the hospitals from being overwhelmed, but that's already happening. If you go to a hospital today with a fever, you'll be shunted into an infectious disease ward, where they might put you on a ventilator.
Any new drugs would have to go through the FDA's multi-billion-dollar gauntlet of clinical trials and mountains of paperwork before they get approved. Even vaccines will take a year at best. The best hope is to repurpose existing drugs.
Hydroxychloroquine and remdesivir
One promising existing drug, an antiviral called remdesivir, was effective against COVID-19 in one patient, and seven clinical trials are now recruiting. Remdesivir has been granted expanded access status, which means it can be prescribed in the US with permission from the FDA without an IND.
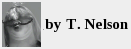
Two other drugs are chloroquine and hydroxychloroquine, which is a less toxic derivative of chloroquine.[1] Chloroquine is approved by the FDA to treat malaria and amebiasis. Hydroxychloroquine was approved in 1955 to treat rheumatic diseases such as systemic lupus erythematosus and rheumatoid arthritis, both of which are autoimmune / autoinflammatory disorders[2,8,9]. Clinical trials for hydroxychloroquine are also recruiting. Both drugs efficiently inhibit SARS-CoV-2 infection in vitro.[3]
For hydroxychloroquine and chloroquine, the 50% cytotoxic concentrations against cultured Vero E6 kidney cells in vitro are nearly identical: 273 and 249 μM. Chloroquine is about 40% more potent than hydroxychloroquine against SARS-CoV-2 in cultured cells, around 2.7 compared to 4.5 μM.[1] This is a small difference in pharmacological terms.
However, chloroquine, which is commonly sold to kill fungus in aquarium tanks, is teratogenic and neurotoxic (LC50=70 μM) (see below). Its principal mechanism of action against the virus is thought to be to raise the pH of the endosome, making it more basic, which inhibits proteases that are essential for SARS-type viruses to infect cells. Thus, it may be acting on the same target as camostat.
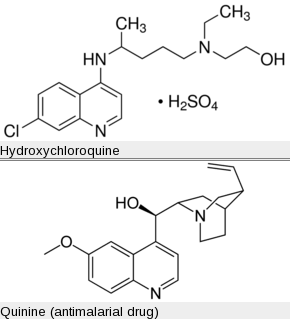
Although quinine and chloroquine are both quinoline derivatives, no anti-SARS viral activity has been reported for quinine. Quinine's effect on malaria is believed to be to cause the buildup of heme inside the malaria parasite cells, killing them. Some researchers have proposed using quinine against HSV-1 and dengue fever viruses.
Update There seems to be confusion on the internet about chloroquine phosphate. Chloroquine is basic (pKa 8.4 and 10.1) and therefore it's usually sold as a salt, which means it's been neutralized by sulfuric, hydrochloric, or phosphoric acid. This means chloroquine phosphate, chloroquine sulfate, and chloroquine hydrochloride all contain the same ingredient.
Cytokine storm
SARS-type virus pathogenicity is associated with cytokine storm, which is a rapidly fatal immune response that occurs in toxic shock syndrome and septic shock and leads to multiple organ failure.[5] Hydroxychloroquine reduces cytokine storm by increasing the pH of organelles in antigen-presenting cells, including dendritic cells and B cells, making them more basic. This prevents the cells from processing the antigen (i.e. degraded bits of virus proteins) and presenting the fragments via the major histocompatibility (MHC) class II proteins to T cells, preventing them from releasing cytokines. It also inhibits TLR-7 and TLR-9 (toll-like receptors 7 and 9), pattern recognition receptors that induce more cytokines.
What this all means is that hydroxychloroquine and chloroquine could be acting against the Wuhan coronavirus in two ways: by inhibiting the proteolysis of the SARS spike protein (which is essential for infection) and by blocking cytokine storm. Either hydroxychloroquine or chloroquine can be legally prescribed for off-label use without FDA approval, though it may be risky to administer chloroquine to a pregnant female.
What is cytokine storm?
Normally an antigen presented on antigen-presenting cells induces both immunostimulatory and anti-inflammatory pathways. Certain antigens, like Staphylococcal enterotoxin B, called superantigens, bypass the anti-inflammatory pathway and induce hyperinflammation and cytokine storm.
Treatments for cytokine storm include high-dose intravenous immunoglobulins, low dose hydrocortisone, and activated protein C. At one time, there was hope that antibodies against TNF-α or interleukin-1 would be effective, but these antibodies failed in clinical trials. Some other proposed treatments include tocilizumab, an antibody against interleukin-6 receptor, and hemofiltration, but these are still experimental. A better treatment is needed.
A disastrous Phase I 2006 clinical trial of an anti-CD28 antibody, which had worked in macaques with no side effects, induced cytokine storm in six healthy human volunteers, leading to lung injury, renal failure, and disseminated intravascular coagulation. Two patients got prolonged cardiovascular shock and acute respiratory distress syndrome. Luckily all six survived.[6] This was a surprise and showed that immunotherapies can be unpredictable and need clinical testing.
Side effects and teratogenicity
Chloroquine can be toxic, causing retinopathy, blindness, brain damage, and death.[4,7] A reactive oxygen species (ROS) mechanism is implied because its toxicity is reduced by substances like ascorbic acid and reduced glutathione that deplete oxygen radicals. In rats chloroquine causes birth defects including enlarged liver, cleft palate, wrist drop, clubbed foot and brain liquification.
Hydroxychloroquine can cause vomiting and diarrhea. High doses over five years can cause retinopathy. Hydroxychloroquine is less teratogenic than chloroquine.
ACE2
Hydroxychloroquine and chloroquine are also said to inhibit glycosylation of ACE2, which is to say they prevent the ACE2 protein from getting a sugar molecule attached to it. It's been suggested that this might be another way hydroxychloroquine and chloroquine can reduce the severity of COVID-19.
SARS-type viruses must bind to a protein called angiotensin-converting enzyme 2 (ACE2) in order to enter the cells. Some countries use ACE inhibitors to treat hypertension; these drugs have the side-effect of increasing ACE2, which would allow more virus to enter and make infection more severe. It's been reported that 99% of the COVID-19 fatalities in some countries were among patients being treated for hypertension or diabetes. Thus, it is NOT age alone but medical treatment for aging-related diseases that predisposes them to severe illness. Switching patients to a different drug might be a reasonable precaution. They would get a mild illness instead, even if they were elderly.
Update, May 15 2020 Several studies have now been done on this hypothesis. Most but not all have found that there is little or no risk to ACE inhibitors. Most physicians would recommend not changing your blood pressure medication.
What does science need?
Unpreparedness causes panic. We know of diseases that will kill over 100 million people. This is a fact, not a hypothetical computer scenario. We must prepare for them and put a greater emphasis on research into their pathogenesis so a cure is available when we need it. If we wait until the situation is an emergency, we will panic again and the next crisis will hit us much harder.
What does science need? We're being whiplashed by rapidly changing fads in funding priorities from the NIH. We lost a brilliant young researcher last year because NIH wasn't interested in basic research on pathogenic mechanisms in his cultured cells—instead they wanted experiments using astronomically expensive pieces of equipment and trendy clinical trials, which young researchers can't do. The result was trials that were essentially wild guesses by big cheeses with big academic labs. The trials were ill-conceived and they failed. The PIs knew they were wild guesses, they didn't much care: everyone is just chasing government money. Unless this system changes, American science will soon be surpassed by other countries.
The discoveries listed above are examples of the sort of knowledge that's needed before a clinical trial is worth starting. Here are some ideas on what we can do.
1. Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H, Li Y, Hu Z, Zhong W, Wang M. (2020). Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. Mar 18, 6, 16. doi: 10.1038/s41421-020-0156-0. PMID: 32194981 PMCID: PMC7078228
2. McGonagle D, Watad A, (2019). Autoinflammation and autoimmunity in Hashkes PJ, Laxer RM, Simon A, eds. (2019) Textbook of autoinflammation, Springer, Switzerland, p 700.
3. Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 30(3),269–271. doi: 10.1038/s41422-020-0282-0. PMID: 32020029
4. Weniger, H (1979). Review of side effects and toxicity of chloroquine. Bull. World Health 79, 906.
5. Gerlacha H (2016). Agents to reduce cytokine storm. Version 1. F1000Res 5: 2909. Link doi: 10.12688/f1000research.9092.1 PMCID: PMC5224679 PMID: 28105327
6. Suntharalingam G, Perry MR, Ward S, Brett SJ, Castello-Cortes A, Brunner MD, Panoskaltsis N. (2006). Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med. 355, 1018–1028. PMID: 16908486 DOI: 10.1056/NEJMoa063842
7. Oluleye TS, Babalola Y, Ijaduola M. (2016). Chloroquine retinopathy: pattern of presentation in Ibadan, Sub-Sahara Africa. Eye (Lond). 30, 64–67. doi: 10.1038/eye.2015.185. PMCID: PMC4709532
8. Nishimura H, Strominger JL. (2006). Involvement of a tissue-specific autoantibody in skin disorders of murine systemic lupus erythematosus and autoinflammatory diseases. Proc Natl Acad Sci U S A. 103, 3292–3297. PMID: 16492738 PMCID: PMC1413900 DOI: 10.1073/pnas.0510756103
9. McGonagle D, Watad A, Savic S (2018) Mechanistic immunological based classification of rheumatoid arthritis. Autoimmun Rev. 17, 1115–1123. doi: 10.1016/j.autrev.2018.06.001. PMID: 30213700
mar 24 2020, 7:50 am. edited mar 25 2020 7:33 am. updated apr 01 2020 5:27 am