What are statins
 tatins are drugs that inhibit the synthesis of cholesterol in the body.
Lipitor (atorvastatin) is the best selling and most profitable drug of all time. It
has brought Pfizer US$ 115 billion in sales over a decade. Until it went generic,
the annual revenue from Lipitor was more than the GDP of Nicaragua.
tatins are drugs that inhibit the synthesis of cholesterol in the body.
Lipitor (atorvastatin) is the best selling and most profitable drug of all time. It
has brought Pfizer US$ 115 billion in sales over a decade. Until it went generic,
the annual revenue from Lipitor was more than the GDP of Nicaragua.
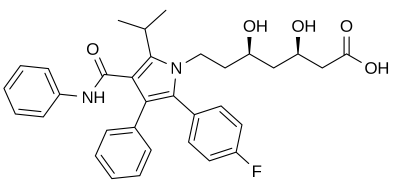
Structure of Atorvastatin (Lipitor)
For years we've been told that statins reduce mortality; if you know somebody who's had a heart attack or who has high cholesterol, you probably know somebody who's on Lipitor. In the USA, 44% of people over 65 and 11% of the overall population are on statins[1,2].
Yet a new study[3] has shown that statins only add, on average, 3 years to your life. Other researchers say the benefits of statins are the result of a statistical trick[4]. The argument here is that if 2% of the untreated group have a myocardial infarction and 1% of the treated group have one, it is not a 50% improvement but only 1%.
It's a good point, but I have to admit I don't find the argument convincing. But there are other potential statistical problems. Along with statins, doctors also give patients stern lectures on diet and tell them in no uncertain terms that they must stop smoking. Patients who've just had a heart attack are in a mood to listen. Statins also may reduce the risk of colorectal cancer, by somewhere between 0 and 43%[1]; but again, patients who are willing to take statins may be the more cooperative ones, and more willing to get a colonoscopy and eat fiber. More investigation is needed to dissect out the psychological from the medical factors.
Pfizer got the rights to Lipitor after buying Warner-Lambert. Any of the former Warner-Lambert scientists, many of whom are now salespeople, cab drivers, and burger flippers, will tell you that Lipitor dramatically reduces LDL-C (low density lipoproteins complexed with cholesterol) in the blood plasma. Statins work by inhibiting HMG-CoA reductase, an enzyme that produces mevalonate. This reaction is the rate-limiting step in cholesterol synthesis.
Like most drugs, Lipitor has its share of adverse effects (AEs) including myalgia, rhabdomyolysis, and in some cases type 2 diabetes. But the one neurologists worry about the most is what's euphemistically called “memory loss.”
Cholesterol and the brain
Very little of the cholesterol that you eat makes it into the brain. Only tiny amounts cross the blood-brain barrier (BBB), so the brain has to synthesize its own cholesterol, which is essential for neuronal function and cell growth. Since cholesterol is a water-insoluble lipid, it can't dissolve well and doesn't float around free in the cyosol as most other molecules do. It is transported stuck to a protein called apolipoprotein E in a molecular complex that's secreted by astrocytes and taken up by neurons, where it acts as a signal for synaptogenesis (the formation of new synaptic connections between neurons), which is an essential part of memory.
This means if a statin gets across the BBB, it could interfere with memory and brain function. For this reason, some people have suggested that statins may contribute to Alzheimer's disease, but the idea hasn't gotten much traction. ApoE/cholesterol is also involved in clearance of beta-amyloid from the brain, so one could hypothesize that a side-effect of statins might be to raise beta-amyloid levels. But they don't; they actually lower them[5,6], and behavioral tests don't adequately discriminate between Alzheimer's and other types of memory loss, so proving a link would be difficult.
Yet such is the popularity of the cholesterol hypothesis that many investigators have tested statins as a possible way of preventing Alzheimer's disease. That didn't work either: statins had no benefit effect on the incidence of dementia as measured by two prominent behavioral tests, ADAS-Cog and MMSE[7]. This should perhaps not be surprising since most statins cannot cross the BBB any better than cholesterol. Simvastatin, a more lipophilic statin, is said to be an exception[8], and it has been proposed that simvastatin actually strengthens the BBB which is damaged by (you guessed it) cholesterol[9]. But then again, caffeine protects the BBB too, at least in cholesterol-fed rabbits[10]. (Rabbits are good models for this because their bodies have almost no fat and they never eat food that contains cholesterol; those nervous coffee-drinking fat carnivorous rabbits exist only in the lab and in the movies).
This is all a roundabout way of saying that cholesterol is much more complicated than many people think. Statins are not perfectly benign drugs, either—they have risks. But if they reduce your risk of dying from cardiovascular disease the risk might be worth taking[11].
Yet patients should be skeptical. In a typical article “Does the use of statins improve outcomes in coronary artery bypass graft surgery?”[12] the authors write:
“The clinical significance of specific statin agent and dose, acute statin withdrawal and the potential benefits associated with statin reloading remain important yet currently unresolved issues. Despite limited high-quality evidence, class I recommendations have been made that all patients undergoing coronary artery bypass graft surgery should receive statin therapy unless contraindicated.”
In other words, as far as coronary artery bypass graft surgery is concerned, they don't help, but they couldn't hoit. ‘It couldn't hoit’ is the position many doctors take; it should be Pfizer's marketing slogan.
Is LDL-C the real culprit?
In 2013 The American College of Cardiology/American Heart Association (ACC/AHA) increased its recommendations for high-intensity statin therapy for prevention of atherosclerotic cardiovascular disease[13]. This more than doubled the number of patients eligible for statin therapy, from 24.5 to 55.5%. Yet in one 10-year study[14], high-intensity statin therapy (that is, doses that reduce LDL-C by more than 50%) induced type 2 diabetes in nearly as many patients as it protected from atherosclerotic cardiovascular disease (ASCVD) events. Patients who have diabetes already would presumably be immune from this risk and so they are more likely to be put on statins[15].
The basic assumption among practitioners seems to be that statins are so beneficial that the benefits outweigh the risks. But in the scientific community there is still a large reservoir of doubt. It seems clear that the presence of high plasma LDL does not by itself cause cardiovascular disease, otherwise statins would have cured it. So what is going on?
There are many possibilities: perhaps white blood cells (leukocytes) or macrophages oxidize cholesterol to produce toxic products like oxidized cholesterol. This would be correlated to cholesterol levels but not intake, since dietary cholesterol seems not to raise long-term plasma cholesterol levels. Or perhaps some microorganism is activated by cholesterol, like those oil-eating bacteria the oil industry uses to clean up oil spills. Statins can also lower the levels of testosterone and other metabolites of cholesterol. These sex hormones are important in the brain, where they do non-sex-related stuff, and are known generically as neurosteroids. Or maybe statins are reducing inflammation. They also interfere with synthesis of isoprenoids such as geranylgeranyl pyrophosphate and farnesyl pyrophosphate[16,17]. Things for scientists to do.
Or—worst case scenario—maybe the literature has once again gotten contaminated by selective reporting, just as it was for decades with the now-debunked claims about dietary cholesterol and saturated fat.
The problem is that the treatment seems to help, but we may be stuck in what psychologists call the intermittent reward syndrome. When a reward such as a food pellet only occurs part of the time, it increases resistance to extinction[18]. Intermittent rewards are more highly motivating than guaranteed rewards. An example is when people check their email continuously for a reward that only occurs at random intervals. The infrequency of the reward reinforces checking all the time. Result: your kid walks into a telephone pole, causing a head injury.
There's a huge literature on philosophy of science. Maybe what we really need is more psychology of science. Otherwise, we might be stuck in a greasy local minimum forever, endlessly pressing that food lever, hoping for a reward that never really comes.
References and Footnotes
1. Lochhead P Chan AT (2013). Statins and colorectal cancer
Clin Gastroenterol Hepatol. 11(2), 109–14.
link
2. National Center for Health Statistics. Health, United States, 2011: With Special
Feature on Socioeconomic Status and Health. Hyattsville, MD: 2012.
link
3. Citation needed
4. Diamond DM, Ravnskov U. (2015). How statistical deception created the appearance that
statins are safe and effective in primary and secondary prevention of cardiovascular
disease. Expert Rev Clin Pharmacol. 8(2),201–10.
link
5. Shinohara M, Sato N, Kurinami H, Takeuchi D, Takeda S, Shimamura M,
Yamashita T, Uchiyama Y, Rakugi H, Morishita R. (2010).
Reduction of brain beta-amyloid (Abeta) by fluvastatin, a hydroxymethylglutaryl-CoA
reductase inhibitor, through increase in degradation of amyloid precursor protein
C-terminal fragments (APP-CTFs) and Abeta clearance.
J Biol Chem 285(29),22091-102.
link
6. Ostrowski SM, Wilkinson BL, Golde TE, Landreth G. (2007)
Statins reduce amyloid-beta production through inhibition of protein isoprenylation.
J Biol Chem. 282(37),26832-44.
link
7. McGuinness B, Craig D, Bullock R, Malouf R, Passmore P. (2014).
Statins for the treatment of dementia. Cochrane Database Syst Rev. 7, CD007514.
link
8. Simvastatin. http://www.alzforum.org/therapeutics/simvastatin
9. Jiang X, Guo M, Su J, Lu B, Ma D, Zhang R, Yang L, Wang Q, Ma Y, Fan Y. (2012).
Simvastatin blocks blood-brain barrier disruptions induced by elevated cholesterol
both in vivo and in vitro. Int J Alzheimers Dis. 2012,109324.
link
10. Chen X, Gawryluk JW, Wagener JF, Ghribi O, Geiger JD. (2008).
Caffeine blocks disruption of blood brain barrier in a rabbit model of Alzheimer's
disease. J Neuroinflammation 5,12.
link
11. Disclaimer: I would never take a statin myself, no matter what
my doctor said. But then, where I live, the only doctors who actually see
patients are residents, which means they only know what's in the textbooks; my job is
to prove those textbooks wrong, which may be one reason why my doctor hates me so
much.
12. McIlroy DR, Myles PS. (2015).
Does the use of statins improve outcomes in coronary artery bypass graft surgery?
Expert Rev Cardiovasc Ther. 16, 1-4.
link
13. Zupec JF, Marrs JC, Saseen JJ. (2015). Evaluation of Statin Prescribing for
Secondary Prevention in Primary Care Following New Guideline Recommendations.
Ann Pharmacother. 2015 Sep 28. [Epub ahead of print].
14. Yeboah J, Sillau S, Delaney JC, Blaha MJ, Michos ED, Young R, Qureshi WT,
McClelland R, Burke GL, Psaty BM, Herrington DM. (2015).
Implications of the new American College of Cardiology/American Heart Association
cholesterol guidelines for primary atherosclerotic cardiovascular disease event
prevention in a multi ethnic cohort: Multi-Ethnic Study of Atherosclerosis (MESA).
Am Heart J. 169(3),387–395.
15. Ades PA. (2014). A controversial step forward: A commentary on the 2013 ACC/AHA
guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular
risk in adults. Coron Artery Dis. 25(4),360–3.
link
16. Kavalipati N, Shah J, Ramakrishan A, Vasnawala H. (2015).
Pleiotropic effects of statins.
Indian J Endocrinol Metab. 19(5),554-62.
link
17. Wang CY, Liu PY, Liao JK. (2008).
Pleiotropic effects of statin therapy: molecular mechanisms and clinical results.
Trends Mol Med. 14(1),37-44.
link
18. http://www.intropsych.com/ch05_conditioning/intermittent_reinforcement.html
